As the 2020 interview season begins to wane, I have noticed a continued pattern among many medical schools. They still consider radiology to be just an “elective.” So, why do medical schools not take the specialty of radiology seriously enough to make it a requirement? Well, I have a few theories. Maybe, they want to limit exposure to medical students to shunt them toward the primary care track. (Yes, they do get government and private funds for doing so!) Perhaps, it’s a bit of inertia that schools don’t like to change. Or, it may take the place of education in other specialties since there is only so much time.
Regardless, they are making a big mistake for several reasons. First, of course, radiology insinuates itself into almost every medical specialty. And then, let’s face it, all students should learn a bit of radiology to be a well-rounded clinician. But, most importantly for society, however, radiology is one of the most expensive cost centers in health care for patients. So, let me give you a few good reasons for why medical schools should make radiology into a requirement instead of an elective and how it increases the cost of patient care.
Incorrect Orders
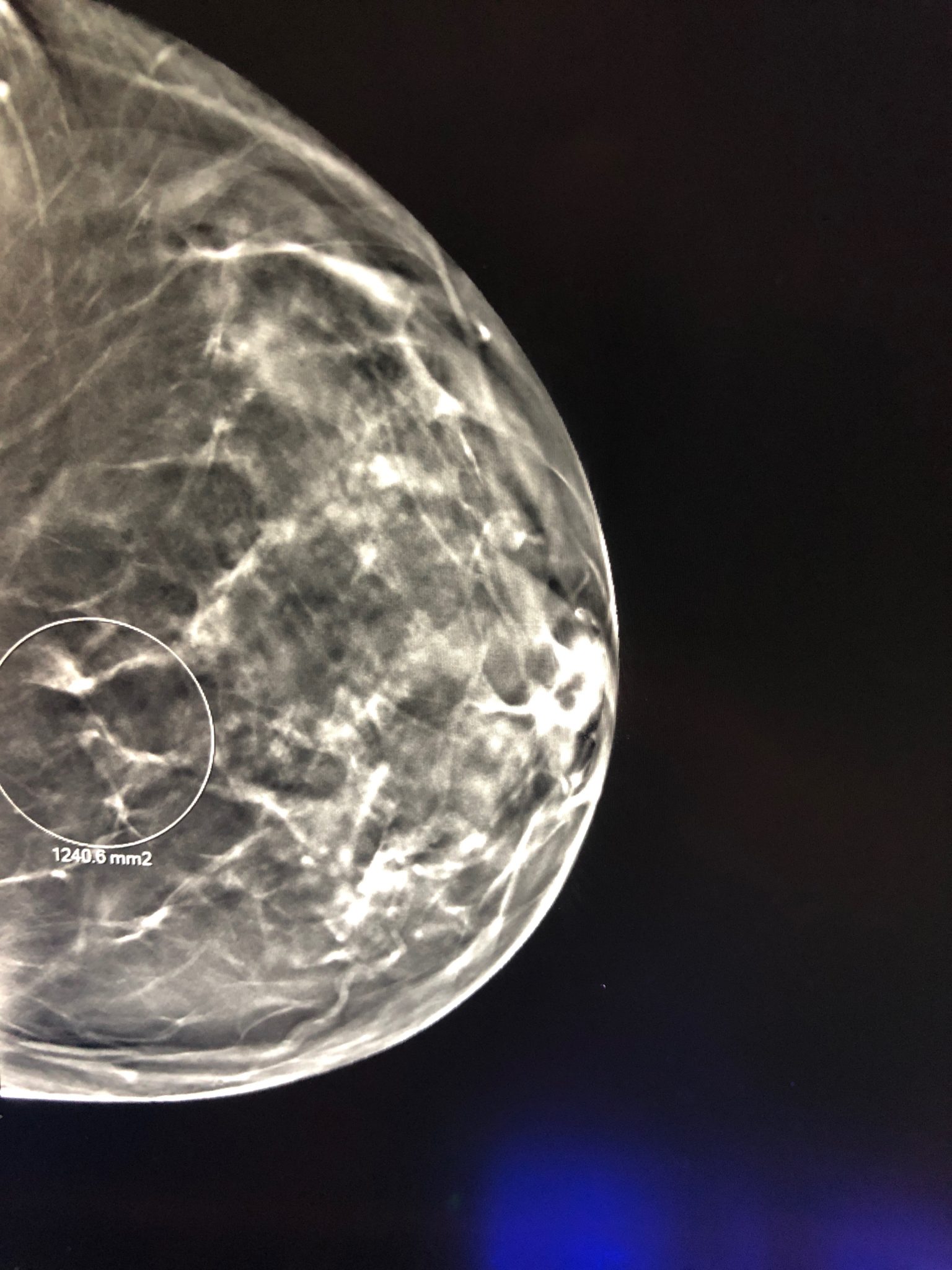
As a radiologist, if you haven’t noticed all the incorrect orders that flow through the system, you are probably living under a rock! Daily in breast imaging alone, I see at least a few ordering mistakes come through the department. For instance, the doctor orders a bilateral breast ultrasound when the patient only needs a unilateral breast ultrasound. Or, a clinician requests an ultrasound of the breast when a mammogram is in order. Sometimes, I can catch these mistakes before the imaging ensues. But other times, the study is completed before I even had time to decide on appropriateness. And, yes, doctors sometimes order these studies incorrectly because they have not had experienced a radiology rotation! Imagine the decreased costs of getting these orders correct?
Repeat Tests
Along with the theme of incorrect orders, clinicians wind up reduplicating their efforts because some don’t know what they are ordering. Let me go back to the example of breast imaging. Typically, we do a mammogram first in older patients when they say they feel a lump. If you do the ultrasound first before a mammogram, you are more likely to have to do two ultrasound exams instead of one. Why? Because you are more likely to find other findings on the mammogram that you will need to image with ultrasound. If the ordering clinician knew this, he would have been much more likely to save the extra test. And, this is just one example among many!
Wrong Disease Pathways
Then, of course, ordering the incorrect test leads to working up incidental findings. You gotta love those incidental findings! Noninvasive imaging is not benign. Why? Because it can lead to invasive procedures. How about that thyroid nodule that you incidentally detect on an unindicated MRI of the cervical spine? Or, you find a benign lung nodule on a CT chest that the doctor should have ordered as a regular chest film. You now need to work it up! All these incidental findings add undue costs to the system!
Lack Of Understanding of Reports
And finally, without adequate training in radiology, you can blow the significance of findings out of proportion or shove them under the rug. For instance, I have reported on a Schmorl’s node in the lumbar spine (intravertebral disc herniation) with little clinical significance. And I have received phone calls asking what to do for the patient with this diagnosis, biopsy, or not! (Absolutely nothing, of course!) Likewise, I have seen patients with new cortically active bone lesions that a clinician may ignore due to a lack of understanding of its significance. Nevertheless, in both situations, the costs of acting or being inactive incorrectly can rapidly add up for the patient and the system!
For The Sake Of Society- Make Radiology A Requirement, Not An Elective!
Unfortunately, these examples are just the tip of the iceberg. Inadequate radiology education as only an elective allows physicians to skip out on radiology in medical school. And, since radiologists do not control the flow of imaging exams, incorrect orders from poorly trained physicians will continually slip under the radar. So, the solution is simple yet bold. Make sure that all medical students receive a basic education about radiology and ordering radiological tests. We will markedly decrease the cost to the health care system and improve patient care. You got that, medical school administrators!