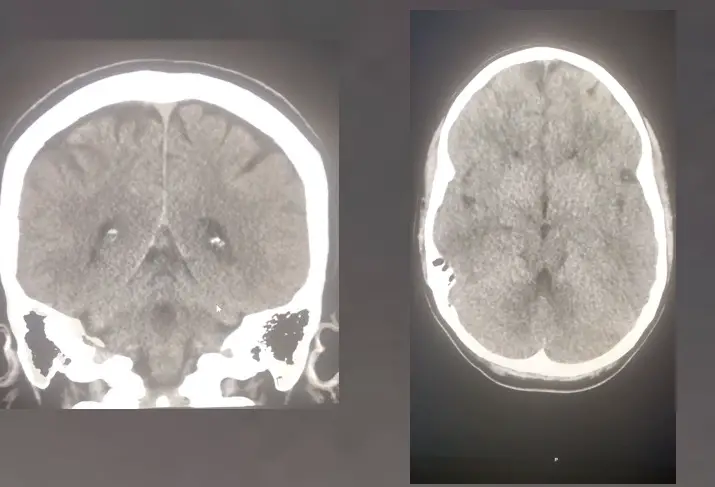
Due to improving CT scanner and software technology, the resolution and detail of reconstructions have dramatically improved over the past ten years. Nowadays, most institutions include these CT reconstructions in their protocols without even an afterthought. However, it wasn’t always like that. And, like most other images from a CT exam that we add onto PACs, these images exist for a good reason.
But, with the increasing numbers of slices, it has become more common to forget about them. And, that’s understandable. It takes extra time to look at so many additional images. So, let’s go through why it’s worth our time to give them a well-deserved second look and why you should not interpret a case without them.
Some Structures You Can Only See In Another Plane
Ever go through a CT scan and search for the appendix? Especially in folks with a lot of intra-abdominal fat, they pop up in seconds. But, in the typical thin child with lots of contrast filled bowel and not much fat, the abdominal axial images do not help all that much. It is the magic of the coronal plane that often lets you see the appendix in all of its glory.
And, it is not just the appendix. I have seen renal tumors with barely a contour defect at all on the axial images. But, when you look at the coronals, they become readily apparent.
What else? Well, compression fracture deformities magically appear on the sagittal images, sometimes without a hint of abnormality on the axials. So, make sure to use these reconstructions wisely!
Increased Conspicuity
And, it’s not just that you can only see some structures on individual planes. Other times, it just becomes a whole heck of a lot easier to make the findings. Take the bowel, for instance. If you go back to one of my cases from May 25, 2019, you can find a colon cancer that was exceedingly hard to pick up on the original axial images. However, on the coronal images, it becomes a bit more reasonable to find. And, this holds for many other organs as well. Liver lesions, lung nodules, and fractures are other examples of findings that can sometimes be much easier to detect in different planes.
You May Miss The True Consequence Of The Finding
On the axial images alone, you can interpret the findings in the wrong way. Take a look at a typical CT scan. Many times diffuse ground-glass opacities on axial images can look entirely linear on a coronal or sagittal. And, that makes an enormous difference in the final interpretation. Linear opacities on a chest CT are not clinically relevant. On the other hand, diffuse ground-glass opacities may mean pneumonia, invoking antibiotics and a call to the doctor to return.
Or, you can easily misinterpret disc disease if you look at it in the wrong plane. I can’t tell you how many times I have seen neural foraminal stenosis that disappears once you look at the right sagittal or reconstructed axial planes. It pays to take another gander at these recons!
CT Reconstructions- Not Just Another Useless Set Of Images!
Unfortunately, reading additional images adds more time to the radiologist’s workday. But, the rewards for reading CT reconstruction series and penalties for missing findings without using them are enormous. So, the next time you see another sequence of reconstructions, do not brush them off as just another set of useless images. Instead, make these reconstructions a regular part of your search pattern for any CT scan study that you read. First of all, you will know to ask for them when they are missing. And finally, you will be glad that you did!