This post is different from most. I am going to discuss my start in this field. By writing about my beginnings, I hope to either help you with your specialty decision or keep you going in your residency if you are still unsure once you have started.
Unlike what you might have thought by reading my blogs, I was not initially gung-ho about radiology from day one. In fact, like many medical students, when I first began, I had no clue. As a student, I planned on going into internal medicine after a stimulating rotation in medical school during my third year. I loved my instructors, the academic discussions, the grand rounds, and the camaraderie of it all. I like to say that if you associate with the right people, any task or job could be fun. And that was what happened during that third-year rotation. The stars aligned. Perhaps, I would complete a residency in internal medicine and become a cardiologist.
My Subinternship
And then, wham! I started my subinternship in medicine, a fourth-year rotation at my medical school. On day one, my resident micromanaged everything. And, attendings loved her because her notes were over three pages long. On the other hand, if you worked under her as an intern or fourth-year medical student, you entered an alternate reality. She could not decide what to do next on the simplest of matters. It could be the difference between Tylenol or generic acetaminophen in a healthy patient. No matter. She could not handle the small decisions. We left unnecessarily late every single day.
Moreover, if you did something on your own, exhibited any independence in a decision, she would stare at you with a frown on her face. And, later that same day, she would go to her attendings complaining about her underlings. So, you would hear about what you did wrong. Ahh, the pain.
But, if that was all, I noticed that I spent more time spending hours on the phone with insurance companies and burnt out attendings than any patient-related matters. Additionally, the patient matters that I did take care of were not intellectually challenging. Instead, I worked with the mundane issues of uncompliant patients or patients complaining about the same problems over and over again (obesity, diabetes) but not doing anything to improve their status. Between my team and the actual work, I realized I could not do this for the rest of my life.
Enter The Radiology Rotation
So, I completed my subinternship depressed that my initial career choice did not fit my requirements for what I wanted to do for the rest of my life. Luckily, I had the opportunity to begin my radiology rotation next early in my fourth year. No, there were no epiphanies/signs from above to let me know that radiology was right for me. (although you would never know that from my personal statement!) Instead, I mildly enjoyed my rotation. Looking at images and making interpretations seemed to be the better option than a life of hell in internal medicine. And, what else was there that I wanted to do at the time? So, I started with the ERAS process to create an application for a residency in radiology. A few months later, I matched at Beth Israel Medicine for preliminary medicine and Brown University for radiology. I was mildly enthusiastic.
Prelim Medicine Year- Second Thoughts
Like many of you out there, as I started my internship year in preliminary medicine, I began to question my original decision to go into the field of medicine in general. As the year progressed, I became even more disenchanted with medicine. My disenchantment eventually bled over to my initial thoughts about becoming a radiologist. Was I making the right decision?
Once again, in the dead of winter, I can remember being in a rotation in infectious disease with another crazed medical resident as my supervisor. This time, he was exceptionally aggressive and irritating. He had reported me to the program director for insubordination. Fortunately, that complaint did not go anywhere. But, it left a bad taste in my mouth. After that situation, I thought about interviewing for financial jobs and even completed one. However, I realized that with the excessive debt that I had from medical school, it would probably not end well. So, I stuck it out and made it through to my first year of radiology residency.
Radiology Residency- A Hellish First Year
Again, you would think that I started radiology, and everything became as smooth as a diamond. But, you would be entirely wrong. I began my residency reading a lot. But, it did not show during noon conferences. Nor did it manifest itself on rotation. As I like to say in some of my other posts, I committed the cardinal sin of reading as a first-year in radiology. I did not emphasize the pictures but instead read through mostly text without the images. So, when it came time to interpret pictures, I was somewhat clueless.
Also, I was not so “procedurally inclined.” One of my instructors (who shall remain nameless!) made sure to make that well-known. He would talk about me behind my back. Instead of helping me to become better, for the first time, I found out about this on an evaluation six months later. To this day, it left a bad taste in my mouth.
As the year progressed, I can remember the faculty’s pressures, not believing that I would be able to perform well on call. Should they even let me? Fortunately, I barely passed the precall quiz. And, my adventures in the second year would subsequently begin.
The Rest Of Radiology Residency- I Could Do This As A Career!
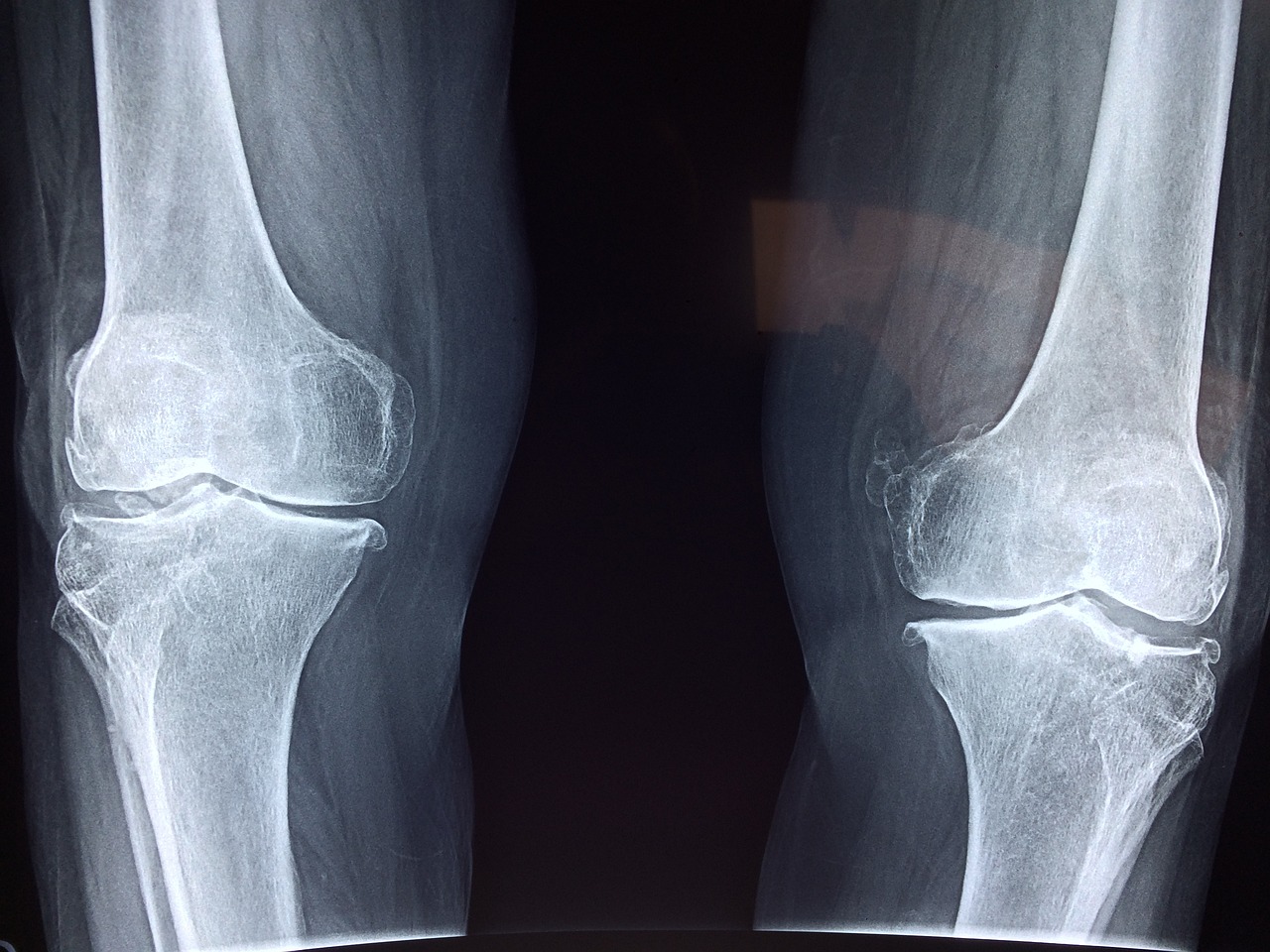
So, when did my outlook on radiology change? My new world order started once I began taking calls at the start of my second year. For the first time, I had some control over the environment. I could make my own decision, and it mattered. Every night, I found that I became more intellectually challenged. With each call, I discovered difficult cases. Even the attendings were unsure about them. And I would enjoy looking at the images and arriving at appropriate differential diagnoses. Finally, I gained the respect of my faculty as a decision-maker and a colleague. I felt part of the team. The rest was history.
So, What Was The Point Of Telling You How I Made My Decision?
Well, I think it is critical that every one of you, whether in medical school, internship, or the start of residency, should realize that you will find a light at the end of the dark tunnel of medical training. Don’t expect that the long road will match your expectations along the way. Having doubts during the process of residency is OK. Nevertheless, try to give radiology a chance and stick it out for the long run. I think that most of you have probably made the right decision for your career. It was an excellent fit for me. And, I believe that if you can persevere, you will find that radiology as a career will reward you as well! Until next time…