Like many institutions, we perform cardiac CTA studies at the behest of our emergency medicine, internal medicine, and cardiology colleagues. They say do the study, with or without a protocol, and the technologists jump without a reflexive thought. For example, one patient had a chest CT scan a few days earlier for shortness of breath. It turned out that the patient had enough calcium in their coronary arteries to make their vessels look like lead pipes. For those who know anything about cardiac imaging and CTAs, tons of calcium within the coronary arteries make it nearly impossible to interpret them for stenosis because of significant beam hardening artifact, limiting evaluation of the lumen.
Nevertheless, without batting an eyelash, the technologists completed the coronary CTA, which was uninterpretable for detecting coronary stenosis. It had a calcium score of over 4400! Now, if only someone had looked at the CT chest, we could have avoided the CTA chest at the cost of unnecessary contrast, additional radiation, and of course, the financial cost to the patient.
This case is a microcosm of what is happening to radiology. Scans come through fast and furious, making it difficult to vet the protocol and the priors on everyone. But, by letting cases get through the system without forethought and protocols, we expose our patients to subpar medicine. In light of these facts, here are some of the critical reasons why radiologists need to protocol cases.
Avoid Unnecessary Studies
How often do we get the wrong orders for the indication? Very frequently! Daily we get orders for CT scans that ask for contrast when none is needed and vice-versa. Of course, a patient with flank pain should not generally get contrast on the first scan if they are looking for stones. But, wrong orders for studies with contrast happen all the time, causing unnecessary exposure to radiation and contrast that is not needed. Protocoling can prevent most of that.!
A Protocol Can Make Sure Studies Are Done For The Right Reason
When technologists and nurses come up to me and ask if they are performing the correct study, the first question I always ask is, “why are we doing the study?” There is a reason for that. We get orders that are not necessarily for the indication that clinicians want. It could be a white blood cell scan for when a simple gallium scan is warranted. Nevertheless, we can correct most of these potential errors before they get to the table!
Protocols Can Add Information To The Case
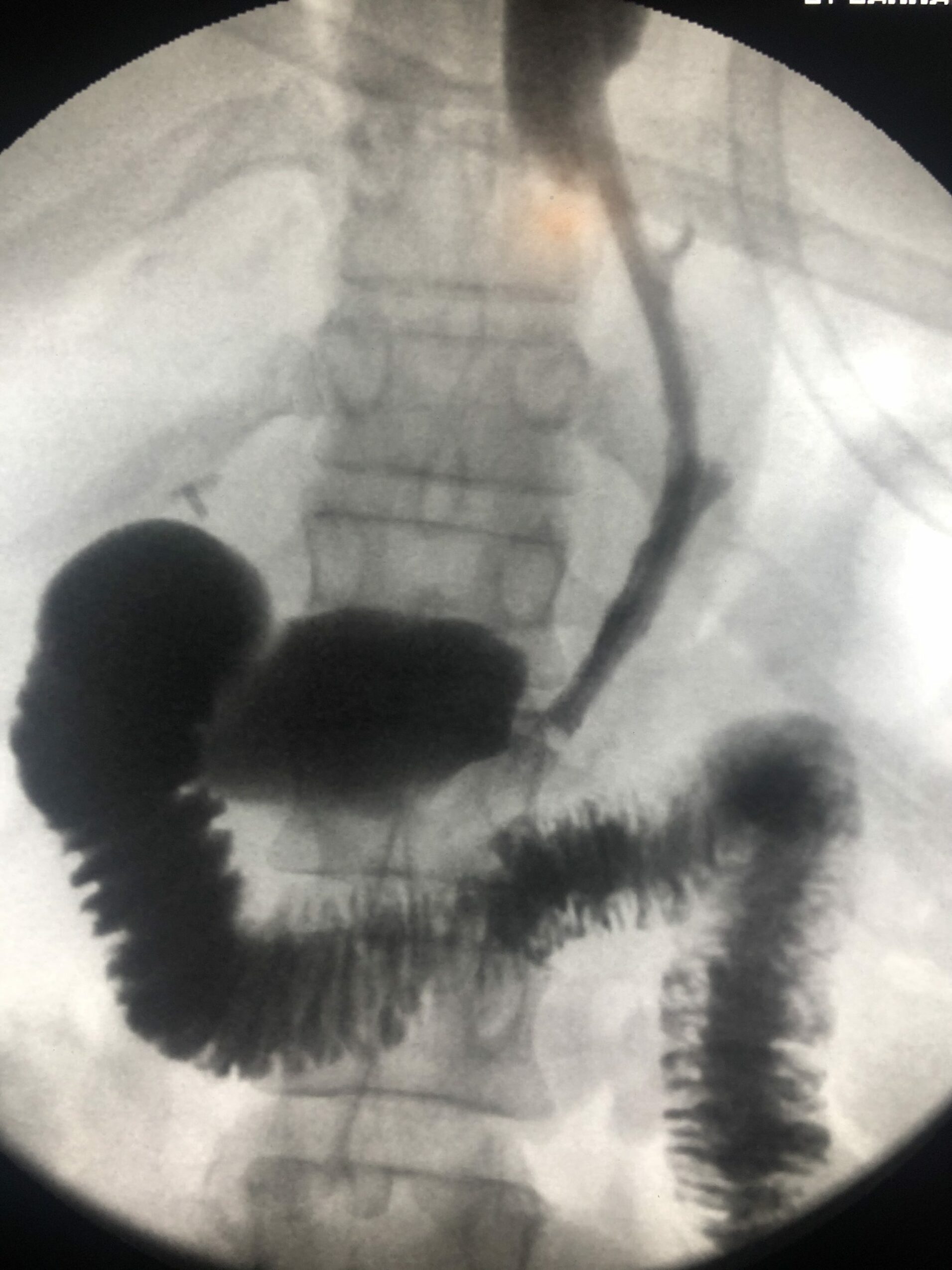
Protocoling can add critical information to the case. It may help find a relevant prior like the cardiac CTA above. Or you might find a valid reason for a study that might not be evident initially. Perhaps, the doctor is looking for a fistula and needs rectal contrast. Sometimes, you can only figure that out by digging deeper. You know what they say… Garbage in. Garbage out!
Prevent Patient Discomfort
Many radiology studies are uncomfortable and difficult. A CT scan on a patient with severe back pain can be a nightmare. Imagine going through a CT scan in this situation when you could have avoided the test if the radiologist had protocoled it beforehand. Well, this issue happens all the time. We owe it to the patients to prevent additional harm!
Prevent Angry Clinicians
When we do not protocol cases before imaging, we do not get the answers that the doctors are looking for. This cycle leads to unhappy referrers that do not receive the intended study. And, we get these irate phone calls afterward. Do you want your clinician to send patients back to your department again? Well, if you consistently deliver the wrong studies for the patients, that will not happen!
A Protocol Can Decreases Costs
The costs to image patients are immense. And simply one incorrect study can cost the patient and the institution thousands of dollars. Protocoling is a tremendous backstop to ensure that health care costs are more reasonable. Sure, we may not have much time in our busy schedules. But, protocoling can certainly decrease costs to the system!
Protocol: An Easy Way To Prevent Bad Medicine
If your attending asks you to take a stack of patients and ensure the protocols are correct, it is not a waste of time. With all the benefits of eliminating waste and practicing good medicine, it is something that we should all do regularly. So, look at those orders before the hospital performs the studies. Protocoling can make a huge difference in patient care!