Many hospitals and imaging centers throughout the country have recruited radiology residents to help out with the Covid crisis. But that leaves many of these residents in a bind. Some residents may feel that they may be losing some of their hard-learned skills. And many have not had time practicing radiology, the main point of completing their residency. So, I am going to outline some steps to make the next several months more relevant to your training. I will do this by going through each residency year and what you should do to keep up your skills. And, I will divide what residents should into First Years, Second and Third Years, and Fourth Years as each of these groups are in different boats.
First Years
For many first years, you are probably not getting the same case experience as you did before. However, for those of you lucky to have some extra time outside of an ICU rotation, I would go through essential books in each subspecialty section. You will find some ideas for books that you may want to read through in my books and links section of this website. (as recommended by my residents) Make sure to read through some of the recommended reading materials at home, now that you may have more time (or even if you don’t!) The key to a successful first year is reading as a basis for the rest of your residency. Don’t squander this opportunity.
Also, if you are interested in interventional radiology, I would recommend participating in some of the procedures that a clinical rotation like the ICU may offer. Volunteer for lumbar punctures, central venous lines, and paracenteses, if possible. These are some procedures that overlap with radiology and will help to maintain what you have learned.
Second And Third Years
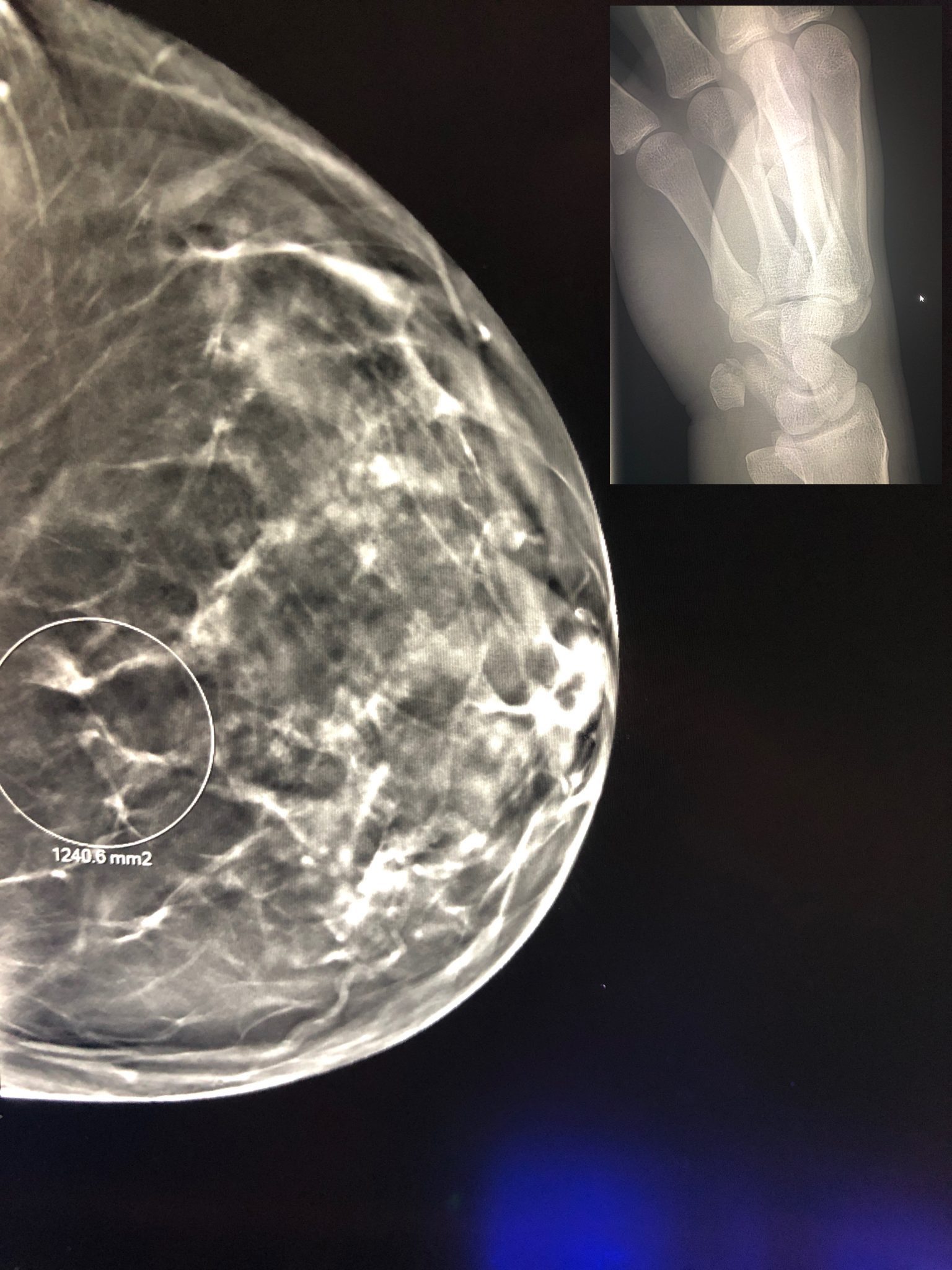
Second and third years are years to practice and learn the art of Radiology. So, in addition to reading like the first years. I would make sure to emphasize radiology cases over only reading raw reading materials/textbooks. So, make sure to go through the case series. Also, when you have the chance, go to the PACS systems and review older cases from the year in different subspecialties, now that some of the regular imaging volumes have dried up. For instance, pick up some of the earlier MSK MRI and make your interpretations and match them up with the final dictations. This action will help to keep your skills and search patterns fresh in your mind since many elective sorts of cases have probably dried up a bit.
Also, even though the ABR has delayed the core examination, it is likely at the forefront of your mind. Make sure to continue to review test questions from sources like RadPrimer and others. (Check out a great post called Up To Date Book Reviews For The Radiology Core Examination from a former resident for some ideas) You certainly want to reinforce this information when you do take the test. Rinse and repeat as much as you can.
Fourth Years
Finally, we need to talk about the fourth year separately. Fourth-year is the best time to learn practical radiology. So, during this time, you should be reviewing areas of practice that you may feel less comfortable with. Especially now, more than ever, I would recommend doing this since the job market will most likely be changing. (Check out my recent post What’s In The Cards For The New Radiologist Job Market After Covid?). So, make sure to read cases in your weaker subspecialties to keep up or learn new imaging skills. (PACS is a godsend!) You may be using some of these skills at your next job!
Keep Practicing Radiology Skills: You Have Worked Too Hard To Lose Them!
Just because some of your radiology training has been canceled does not mean that you should stop practicing radiology. Now, more than ever, you should be making a concerted effort to hone your skills. Whether you are just starting as a first-year radiology resident and need the basics, or if you need more practical training in your final year, allowing your reading and procedural abilities to slip away would be a shame. Reading books and reviewing cases on PACS now is vital. Even though you may be busy outside of radiology with Covid patients, make a concerted effort to stay in the game. Don’t lose your hard-earned skills!
Radsresident is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com