Heraclitus, a Greek philosopher, has been quoted as saying, “change is the only constant in life.” And that concept also extends to how radiologists should commit to a search pattern. Yes, I have stated that you should affix your search patterns so that you make sure to remember to go through all parts of a study. Of course, we don’t want to forget about the images and organs that we need to report. However, every once in awhile the tide changes and we do need to modify our search strategies to incorporate new information.
Sometimes, protocols change. And other times, how you report disease can vary. Now, that does not mean that you should entirely forego your old search pattern. Instead, you can consider adding the new concept to your old one. Based on this thought process, let’s give you some examples of how and when I have accommodated a new change in my search patterns over my career lifetime. Hopefully, these modifications will provide a better idea of when you should make the change as well.
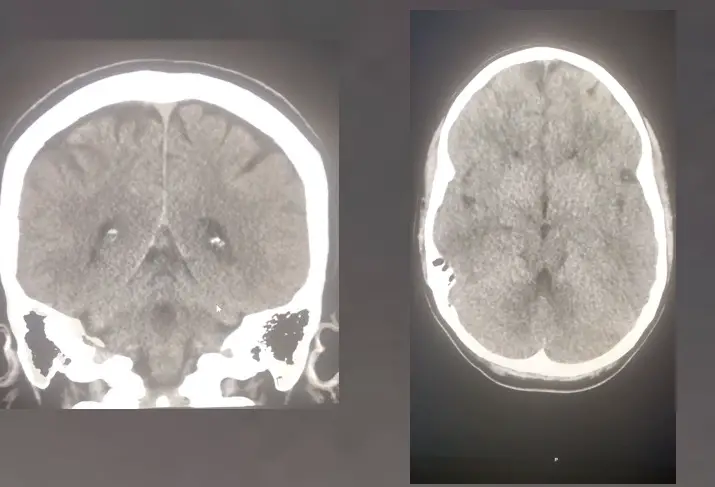
Coronal/Sagittal imaging
Believe it or not, CT scans at one time were only imaged and reconstructed in the axial plane. In fact, there was a big uproar when we decided to add these images to our studies. The techs, administration, and radiologists said there would be too many images to look at and store. But, it turned out that these reconstructions are critical for the interpretation of CT studies. Often, the appendix only shows up well on the coronal images. And, you can have a challenging time catching many sorts of vertebral body fractures on the axial view. Additionally, I’ve seen a few renal and colon masses that you could only pick up on the coronal view. Scary stuff if you decide to neglect these reconstructions.
So, like most radiologists, I had to add these recons to my search pattern to improve my sensitivity for picking up disease. And, this also goes for other sorts of studies. Remember, different planes can be helpful on MRI to catch glenoid labral tears. So, I no longer neglect the reconstructed images and have added them to my search pattern!
TI-RADS
I figured I would also add an example of a required reporting change that had changed my search patterns for a thyroid ultrasound. Previously, I would only make a brief description of a thyroid nodule’s size and cystic/solid consistency. Now, knowing more characteristics that make thyroid nodules more suspicious for thyroid cancer, I incorporate these findings into my reports. In my mind, I run through all the attributes of each nodule using TI-RADS criterion so that I don’t miss critical descriptors. Unfortunately, in the interest of time, I can’t always put a TI-RADS rating for each nodule. But, all the nodules have the description needed for the clinician to make that assessment. New reporting systems will often change how you look at and report the images.
“New” Techniques- Diffusion-Weighted Sequences
And, finally, as an example, new techniques and sequences can also alter your search patterns. They force you to look at new images that you had not seen before. In that regard, the diffusion-weighted technique was a game-changer for acute infarct imaging. Naturally, I always look at them first before any other to make sure patients have no acute infarct. Before the advent of this sequence, our sensitivity for detection of acute ischemia was much lower. Anytime a new technique helps with improving patient care; you need to incorporate it into your search pattern.
“Change Is The Only Constant In Life”: An Application To The Search Pattern
Like this great quote implies, we, as radiologists, cannot rest on our laurels. We need to go with the flow to improve patient care. So, when you have new ways of looking at imaging studies that help with diagnosing or treating patients, make sure to add it to your search pattern. Whether it be, different reconstructions, changing reporting systems, or entirely new techniques, our patients will be better for it!