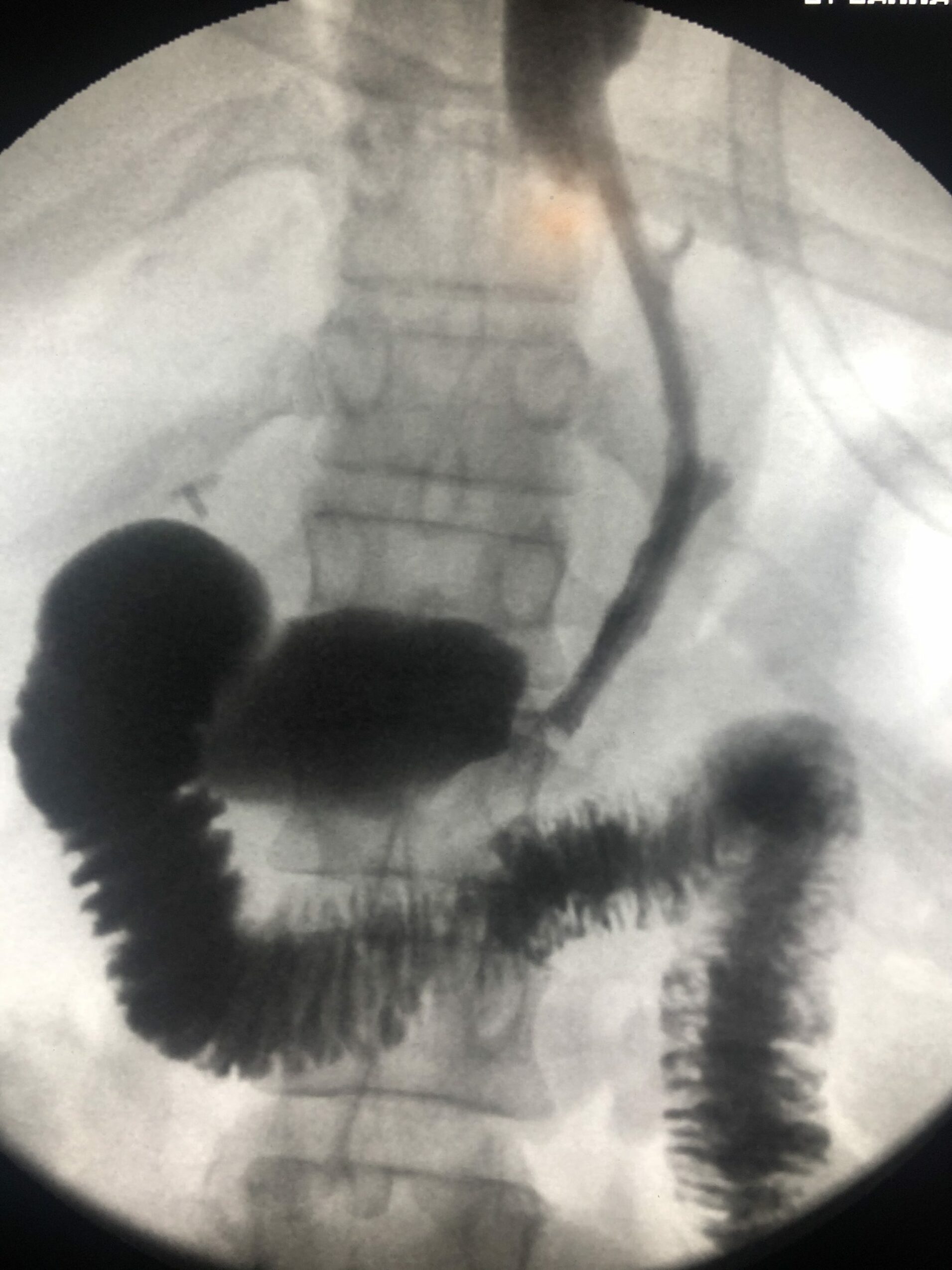
In the second part of the “how to be successful” series, we will walk you through the ins and outs of the breast imaging rotation. Breast imaging, in general, is much different than almost any other area in radiology. (except for some interventional radiology) Why? Because the whole subspecialty hinges on management instead of differential diagnosis. Differentials are usually relatively limited and easy to remember. The challenging part of becoming successful in breast imaging is deciding what to do next. (As long as you don’t miss the finding!)
Also, there are multiple shades of gray in this area of radiology about how to manage patients appropriately. And, it takes a whole heck of a lot of experience to get good at it.
In any event, just like last week, let’s run through what you should read, what and when you should study the appropriate topics, and then finally how you should tackle learning for each year that you are on the breast imaging rotation.
Reading
First of all, I would highly recommend that you check out the free material from the ACR BIRADS atlas on the web. Here, you will get the most up-to-date resource to understand how we dictate breast imaging cases. Additionally, you will learn the appropriate semantics for all sorts of calcifications, masses, etc. I would also advise you to look for a copy of the paid atlas to see each of the different descriptors and associated findings. (see if you can find one lying around in your residency program because they cost 250 dollars!) These sources are the best way to understand the mechanics of reporting breast imaging modalities.
Furthermore, you should also have a supplemental reading to understand the rest of the gritty details about breast imaging. My residents have recommended Breast Imaging, the Requisites (I am an affiliate of Amazon for purchases when you click on the link) to do just that. Although reading during this rotation is required, it is a little less critical to function as well than some of the other radiology areas because it is so “experience-based.”
When To Study Topics In Breast Imaging
First-year
During the first year of breast imaging, I would recommend that you stick to reading out mostly screening and diagnostic breast imaging cases while reading the above resources. Why? It would help if you got acquainted with the basics of breast imaging. The basics include positioning/views, artifacts, searching for findings, and breast imaging’s basic mechanics. Try to hold off on doing too much interventional breast procedures until you are well acquainted with the imaging. You can check out a few to get your feet wet. However, the interventions may not make as much sense because most radiologists make the initial screening and diagnostic imaging findings to get to the intervention point. And, you need to understand these modalities first. You will benefit a lot more from understanding all the interventions better later on.
Second-year
Toward the end of your first rotation or beginning of your second rotation, try to be the initial reader on diagnostic mammography cases. Be in the position of deciding on the additional views and then run it by your attending. In mammography, the only way to learn is to handle parts of the cases yourself. If you don’t take charge, you will miss a good portion of the key to breast imaging- management. Also, be sure to enter the ultrasound room for all the breast ultrasound cases possible. Scanning patients will help you learn how to find lesions and what to look for when you find a mammography lesion.
Final residency years
For your subsequent months of mammography, you should make sure to learn how to perform stereotactic breast biopsies, needle localizations, and ultrasound guide breast biopsies. Also, this is the appropriate time to learn the basics of breast MRI. Breast MRI has become an integral part of imaging in the breast imagers arsenal. You need to understand its place and the basics of how to read them. Again, check out the ACR-BIRADS book for the reporting of MRI findings.
Finally, during your last year of mammography, learn all the new “fancy-schmancy delancy” add-ons. Learn about breast MRI biopsies, PEM imaging, or other modalities that may be unique to your institution. At this point, you want to fill in the blanks. Also, make sure that you have a mammography rotation during your fourth year of residency because the mammograms you read count toward MQSA requirements when you start reading mammograms after a one-year fellowship.
How You Should Learn Breast Imaging As A First Through Fourth Year Resident
More so than other specialties, breast imaging is not a “spectator sport” (a quote from my former chairman during my residency!). It involves being proactive in getting the experience that you need. Moreover, there have been a host of studies, specifically for mammography, that show you need to read tons of images to become an expert in breast imaging. So, you will have to be aggressive to get the numbers that you need to be successful in breast imaging. Not all residencies provide the same training in mammography, and some have significantly fewer cases than others. Therefore, this is a critical piece of the pie that you will need to become a consummate breast imager.
The Basics Of Being Successful In Breast Imaging
To summarize, what are the critical factors in learning how to become an excellent breast imaging resident and future attending? Ensure that you read the BIRADS atlas and a supplemental book such as Breast imaging, the Requisites. Start with reading screenings, ultrasounds, and diagnostic mammography. Then, when you are ready, take charge of your cases independently. Perform and learn about interventional procedures a little later. Then finally, fill in the blanks during the final years.
Also, I cannot repeat enough how important experience is for the breast imager. Writing down that you have seen “x” number of cases is not enough in the world of mammography. Make sure that you are looking carefully at each breast image. It is only with experience that you will feel competent enough to become a breast imager when you complete your residency. And, the best breast imagers have seen tens of thousands of cases!