Barium slinging is harmless, right? I mean, what’s the big deal about letting a patient go after you complete a standard esophagram or barium enema? How often have you, as a resident, completed one of these studies without checking the results with your attending, only to let the patient go home right afterward? I bet most of you have done so at one point or another. If there is any complexity in the case whatsoever, I would think twice before letting the barium patient leave before checking it. Why? Well, for lots of reasons. And I will divide them into the following broad categories, legal, lack of experience, extra scrutiny, patient-related issues, and lack of insight into history. Let’s go through them one by one.
Legal Issues
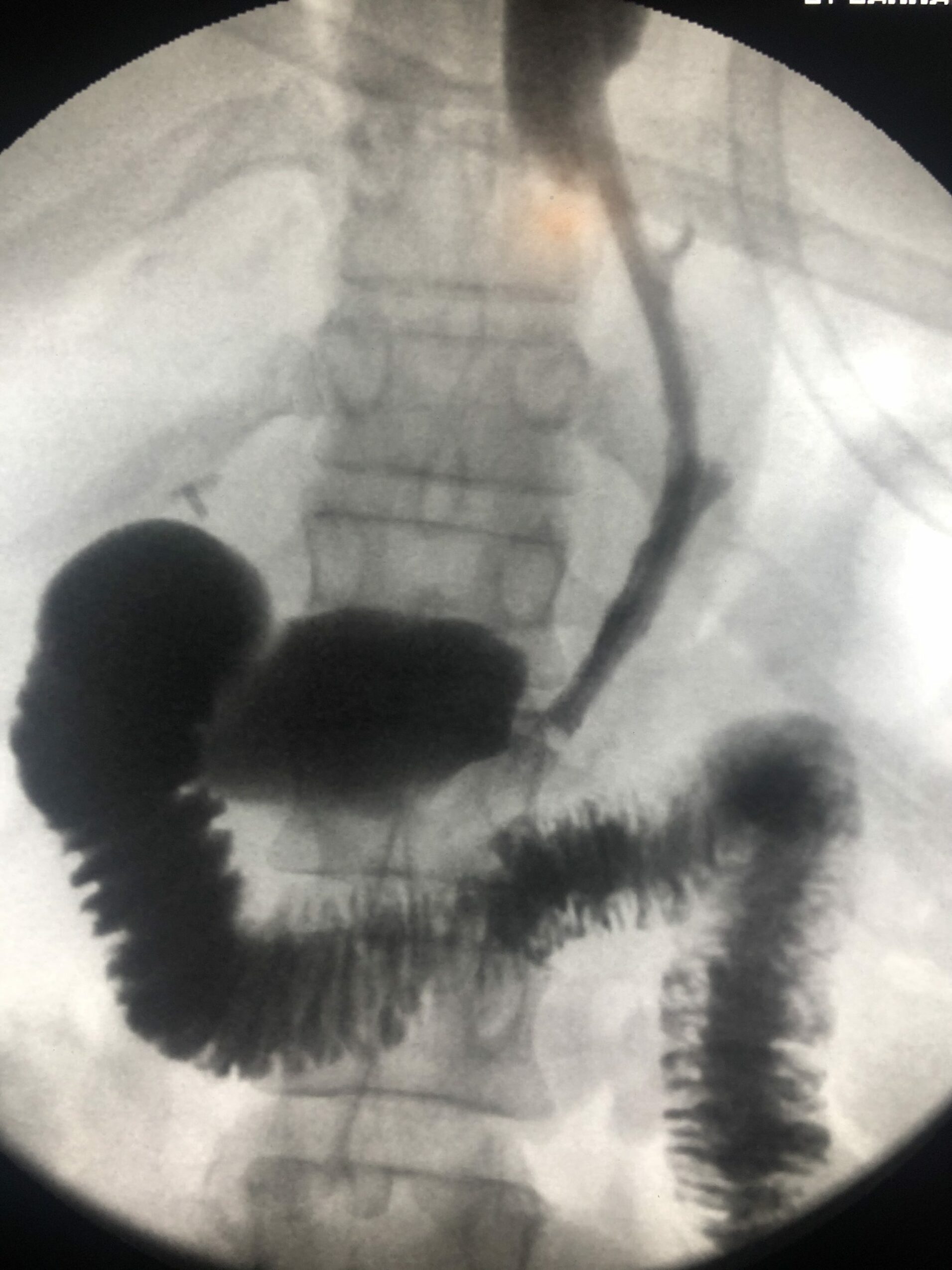
Residents are not the final interpreters of any study, whether it be a plain film, CT scan, or ultrasound. Additionally, distinct from most other imaging modalities (except for ultrasound), the resident is responsible for showing and carefully examining the findings. If she does not technically demonstrate the findings based on history, the study becomes useless to the ordering physician. Consider the resident not spotting the terminal ileum in a small bowel series for inflammatory bowel disease. Or, maybe he doesn’t complete a cine of the upper esophagus in a patient with dysphagia. Who is responsible for the lack of information targeted to patient history? The attending, of course! Just read this AJR article about barium enemas and malpractice, and you will think again. Radiologists are liable for the missed interpretation based on resident imaging!
Relative Lack Of Training
When barium slinging was more common years ago, it used to be one of the more litigious radiology areas. Just like mammography, you could easily miss all sorts of colon cancers, ulcers, and more. Typically, it would take years of experience to develop the trained eye to find these abnormalities. Don’t think that barium work is easy, so much so that you can blow it off as a low tech waste of time. On the contrary, one inexperienced resident may not be enough to catch the pathology that you will need to find. There is hubris in thinking you know more than you do! Moreover, think of this opportunity to go over the case as an additional learning opportunity to become better.
Second Set Of Eyes
On that same notion, having a second set of eyes can be a critical adjunct to making the finding. It’s like breast imaging. Often, the ultrasound technologist cannot find a blessed thing corresponding to the patient’s lump. But, as soon as you, the physician, walk into the room, WHAM! It’s right in front of your face as clear as day. Sometimes, you need that second set of eyes to get you out a particular mindset. It’s worth it.
It’s A Big Deal To Bring The Patient Back
Finally, if you miss looking for a finding on the study, the patient may not return so quickly, especially as an outpatient. For instance, in the patient population with dysphagia, many of these patients may come from rehabilitation facilities or nursing homes. Did you ever think about how hard it was to get the patient to the study in the first place? Or, maybe the person has a hectic job and made special arrangements to complete the procedure. Now, you need to bring the patient back. You may not think so, but it can become a huge issue!
Check With Your Faculty Before Letting The Barium Patient Go!
Don’t take these studies for granted. Allowing for these studies to go unchecked can cause all sorts of trouble, including legal dilemmas, missing findings, and having to bring unavailable patients back for more imaging. So, please, if you are on the fence, think twice before sending that patient home without having your attending check it. It could be lousy patient care!