Yes. Covid-19 has been an epic disaster. But, in any emergency, opportunities arise. And a new Covid surge is no exception. Sure, the hospital may curtail or delay some of your training in radiology. However, this pandemic affords you other chances to establish a reputation for yourself in your hospital and community. And, you will learn other clinical skills that are just as critical as radiology. Demonstrating your prowess in these dark times can lead to unforeseen possibilities in the future. These opportunities can prove themselves more valuable for your future than you might think at first glance.
So, what are these potentialities that I am referring to? Your experiences and performance during the Covid era can lead to job openings, better recommendations, networking, improved clinical skills, better awareness of the community, and more if you play your cards right. Let’s talk about how.
Increased Contact With Hospital Administration
In a typical environment, most residents have very little to do with the hospital administration. At the beginning of the first year, they may hear a few words from the executives to introduce them to the hospital. And at the end of the last year, they help to hand out the diplomas. That’s about it. But, in many departments, this paradigm has shifted.
Now that you are providing a service for the hospital under extenuating circumstances, you are more likely to have the ear of the administration. If you ever want to start looking for a job in the hospital and perform well, they will more likely remember you when the time comes to search. Even better, if you ever want to look for a career in hospital administration, there is no better time to prove your worth and team-building skills than now.
Better Recommendations
Tough times call for more teamwork. And, what better way to get to know your attendings than a stressful situation such as this? In actuality, faculty are more likely to get to know their residents when you are in close contact. You are no longer just another resident! And, this will show in the recommendations that you receive.
Increased Intra-Departmental Networking/Learning
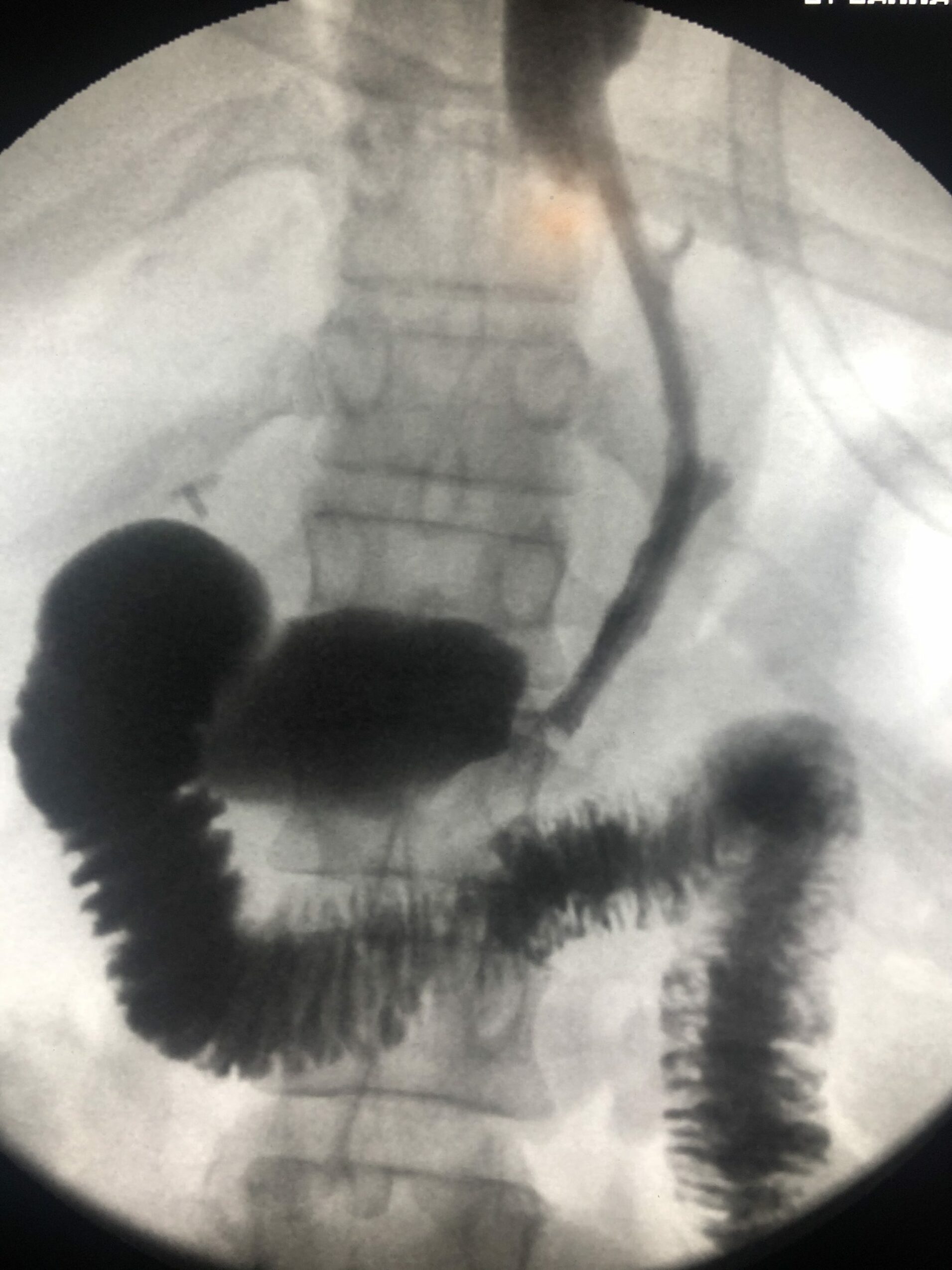
Since you will most likely work with different teams of subspecialty physicians throughout the hospital during a covid surge, you will get to know your colleagues better. Believe it or not, cross-currents of learning and insights into other specialties also help with becoming a better radiologist. It could be pulmonary, cardiology, or pathology. All subspecialties overlap with ours!
Just as critical, establishing relationships with other physicians that you would never have seen as a radiology resident, will make you more valuable. Who would other physicians instead refer patients, a radiologist that they know well, or someone else?
More Awareness Of Clinical Medicine
Sometimes in radiology, we can grow farther away from the real reason why we went into medicine in the first place, to help patients. Having more direct interaction with patients, even in an unforeseen emergency such as this one, can lead us back to our clinical roots and remind us why we are radiologists in the first place. It allows us to rehone our clinical skills that will come in handy later on as an attending.
Getting To Know The Community
Some residents go to residencies based on the quality of the program alone, ignoring the community. However, you also serve a community, and sometimes getting into the clinical nitty-gritty can allow you to understand the patient populations for which you work. If you doubt the importance of your role in helping out the community, look at the media presentation of healthcare workers. Typically, they present all of us (even radiologist residents) serving the hospital as heroes. Heck, in our community, the leaders hosted a parade for the folks at the hospital to demonstrate their appreciation. So, if you think that you do not influence the community, you are dead wrong. Getting back to these roots will allow you to appreciate once again where you work!
Time To Prove Your Mettle During A Covid Surge!
I know. You may not have bargained for these circumstances. However, there are always a few golden nuggets that we can take away in almost any bad situation. So, even though you think there is no value to having work other roles in a surge, it may be more helpful to your career growth than you think!